A heavy problem
Lead standards must be updated to keep workers safe, experts say
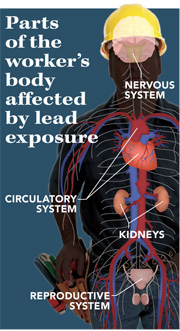
Scientific reports over the past three decades have identified lead as a health hazard. Elevated blood-lead levels have been associated with adverse effects on kidney, nervous system, reproductive and cardiovascular functions. At very high levels, long-term exposure to lead can cause seizures, coma and death.
Because of its ease in casting, high density and low melting point in industrial applications, lead continues to be used in occupational settings across the country. According to the Centers for Disease Control and Prevention, in 2009, approximately 95 percent of all cases of elevated blood-lead levels among adults in the United States were work-related.
OSHA’s Lead Standard (1910.1025) sets the permissible exposure limit at 50 micrograms per cubic meter of air averaged over an eight-hour workday and the highest acceptable blood-lead level for workers at 40 micrograms per deciliter. The Department of Health and Human Services recommends reducing the acceptable blood-lead level to less than 25 micrograms per deciliter for all adults. However, recent research has linked blood-lead levels lower than 25 micrograms per deciliter to health problems, and some experts say occupational practices and standards on lead exposure need to be updated.
Workplace risks
Workers commonly are exposed to lead when handling lead-containing powders, liquids or pastes; through the production of dust or fumes when working with lead-containing solids; or when dry-sweeping debris that has lead in it, according to a report from the NIOSH-funded Adult Blood Lead Epidemiology and Surveillance program.
In 2009, the industries with the highest numbers of employees exposed to lead were manufacturing, construction and mining. Operations with high levels of exposure include battery manufacturing, secondary smelting and refining of nonferrous metal, and painting and paper hanging.
“The key issue is that we [still] have lead exposure in the workplace. We have people with an elevation of lead in their blood levels, and there is a need to work with painters, workers, employees, [etc.], to implement more preventative measures,” said Dr. Walter Alarcon, project officer for ABLES.
Low levels of exposure
Alarcon said reducing blood-lead levels to less than 10 micrograms per deciliter would be safer for employees. Others question whether such a reduction would be enough.
“Lead remains a significant health concern, even though specific programs have been made to reduce exposure,” said Dr. Andrew Rooney, senior health scientist in the Office of Health Assessment and Translation at the National Toxicology Program, a branch of the Department of Health and Human Services. On June 13, NTP released a prepublication copy of a report on the health effects of blood-lead levels in people.
“There’s a considerable body of evidence that adverse health effects are associated with blood-lead levels below 10 micrograms per deciliter in adults and children,” Rooney said. The report, for which he served as lead author, indicated that “eliminating all lead exposures for our environment is our best course of action.”
Update urged
OSHA’s lead standard has not substantially changed since the late 1970s and is based on outdated studies, according to a report from the Washington-based Association of Occupational and Environmental Clinics. “There is an urgent need to revise them,” the report stated.
Travis Parsons, senior safety and health specialist for the Washington-based Laborers’ Health and Safety Fund of North America, said OSHA’s permissible exposure limit for lead must be lowered, and more stringent cleanup procedures should be established.
“The current OSHA regulation is inadequate, as far as we’re concerned,” Parsons said. “There are studies out there that show as low as 5 micrograms per deciliter create the neurotoxic problems.”
Parsons said the NTP draft report is strong evidence that steps must be taken to amend current practices, despite the difficulties in the process.
“OSHA has to walk a fine line there. They have to please a lot of people. There are a lot of things that are hazardous in our lives, so it’s a struggle with any issue to get OSHA regulations, to get any changes or new standards,” Parsons said.
In California, the state’s Department of Public Health submitted revisions of the state’s general industry lead standards to the Division of Occupational Safety and Health in June 2010 and revisions to the construction standards in April 2011.
The department recommended that workers be removed from the lead exposure if a single blood-lead concentration is at or above 30 micrograms per deciliter or if two successive blood-lead concentrations measured over a four-week interval are at or above 20 micrograms per deciliter. DPH also recommended increased medical surveillance and a reduced PEL. At press time, Cal/OSHA was conducting a series of advisory committee meetings to gather stakeholder input into the revised lead standards.
Focus on construction
In the construction industry, old buildings, houses and residential areas are a problem, as they expose workers to lead when metal structures are torn down, renovated or repainted, Parsons said. Bridgework also is a concern because “any older bridge you see out there has lead-coated surfaces,” he said.
“It’s much harder to control the exposure [in the construction industry] because your work environment is constantly changing,” said Scott A. Henn, an industrial hygienist at NIOSH who has studied lead exposure. “In the construction industry, your site changes from week to week. You may be in a different state at the beginning of the day; you could be in an open environment; and at the end of the day, you could be in a closed structure,” Henn said.
“Lead has been a known hazard for quite some time … so it is a problem,” Henn said. “We’re controlling it better; we’re making it more known, but it’s still coming up and it’s not going away.”
Preventive measures
“There are certainly things employers can do to limit lead exposure,” said Dr. Raymond Meister, public health medical officer for the California Department of Public Health Occupational Lead Poisoning Prevention Program. “In the optimal setting, lead will be substituted with something without toxicity,” Meister said. “Then you’ve just eliminated the lead exposure problem.”
Simple changes to a plant, including the machinery, production processes, equipment and work practices, can reduce the dangers of lead exposure, he said.
Certain engineering control tools can isolate lead hazards and reduce the amount of lead a worker is exposed to, Meister said. For example, wet hand-sanding or an electric sander equipped with a high-efficiency particulate air-filtered vacuum attachment could be used instead of dry sanding, he said.
“To prevent workers from being in the situation where they are swallowing lead, provide clean eating areas and wash-up facilities where a worker can wash up their hands, arms and face,” Meister said. “This will help ensure lead dust is not accidentally ingested. Smoking or carrying cigarettes where lead dust is present is very hazardous. Employers must provide appropriate facilities.”
Respirators, coveralls, gloves and other personal protective equipment also will help protect workers from lead, Meister said.
Symptoms of overexposure and treatment
According to the Association of Occupational and Environmental Clinics, once lead is absorbed into the body, it can be found in all tissues. Signs that a worker may have been overexposed to lead include reduced motor skills, such as repeatedly dropping items, said Dr. Marc B. Schenker, director of the Center for Occupational and Environmental Health and professor in the Department of Public Health Sciences at the University of California, Davis.
“Depending on the route of exposure, some people have abdominal pain, abdominal cramps, nausea, vomiting – those are all gastrointestinal manifestations of lead exposure. It could be misdiagnosed as a pancreatic [problem], for example,” he said. “Acute exposure to fumes can cause a whole range of things: confusion or sleepiness to seizures and a coma.”
Treatment options for lead exposure will depend on the level and severity of the symptoms, Schenker said. “In general, the longer it’s been developing the longer it takes to treat. If you have someone that has been exposed to lead for 10 years, you’re not going to treat them in a day or two; it’s going to take a longer process.”
One long-term method of treatment is called “chelation,” which involves administering a medication that helps remove lead from the body. But if symptoms are more severe, a person may need hospitalization or more intensive treatment, Schenker said.
“Lead is lead. Identify and remove the exposure is the key principle in any case. You can’t make assumptions. You have to identify the sources: Is it in the food supply, the water, are you breathing it in? All of those have been identified as causes. First thing you need to do is identify the source and remove the source of exposure,” he said.
Take-home toxins
Workers exposed to high levels of lead at work risk transporting lead dust into their homes. And researchers have found that while low levels of lead exposure may be harmful to adults, the risks to children are much greater.
Family members exposed to take-home lead may be more vulnerable than workers exposed in an occupational setting, according to the Workers’ Family Protection Task Force, a committee of health experts from across the country formed to provide recommendations to Congress on take-home exposures.
When you introduce the same amount of a toxic substance to a child, compared to an adult, children will have a higher level of exposure, said Dr. Anatoly Belilovsky, the medical director of New York-based Belilovsky Pediatrics.
“If we want to reduce the second-hand exposures to children of workers, maybe we should start with reducing the first-hand exposures to the worker in the first place,” Belilovsky said.
“It’s pretty much the root of all evil; it’s the root of all exposures. If you stop at that point, you stop at subsequent points. If you follow them into the workplace and you make sure they handle the lead properly in the first place, then you lose the criticality at all the other stages,” he said.
A study by the Advisory Committee on Childhood Lead Poisoning Prevention found that children may suffer from reduced intelligence, impaired hearing and negative behavioral outcomes from exposure to low levels of lead.
In May, the Centers for Disease Control and Prevention lowered the standard definition of lead poising in children from 10 micrograms of lead per deciliter of blood to 5 micrograms.
Hygiene on the job is particularly important because lead can be transferred on clothing, shoes, tools, in vehicles or even in hair, said Travis Parsons, senior safety and health specialist for the Washington-based Laborers’ Health and Safety Fund of North America.
“You should change out of your clothes or wash them separately and then go home with a clean change of clothes, because you don’t want to take that lead home,” said Parsons, adding that cleaning hair, beards and the face is important because lead dust can be found there as well.
– KH
Post a comment to this article
Safety+Health welcomes comments that promote respectful dialogue. Please stay on topic. Comments that contain personal attacks, profanity or abusive language – or those aggressively promoting products or services – will be removed. We reserve the right to determine which comments violate our comment policy. (Anonymous comments are welcome; merely skip the “name” field in the comment box. An email address is required but will not be included with your comment.)

