Create a volunteer first aid response team for your workplace
NSC experts offer 5 things to think about

Whether it’s a worker experiencing shortness of breath, someone falling on the stairs or a machine-related amputation, workplace medical emergencies take many forms.
The minutes between when an incident occurs and when emergency medical services arrive on the scene can be critical. Some employers – including the National Safety Council – have created in-house first aid response teams, made up of trained volunteers, to assist during that gap.
Teams can provide first aid, help with crowd control to give the distressed person privacy, and collect vital signs and other valuable information to give to paramedics and other first responders.
If you’re thinking about establishing a team, here are five things to consider.
Gauge your organization
Emily Prentice, a senior researcher at NSC, has led the organization’s volunteer first aid response team. She and Robb Rehberg, former director of first aid training and program development at NSC, recommend you look at several aspects of your organization to determine the size and scope of your team.
- How many employees do you have?
- What’s the size of your facility?
- How far is your location from emergency services?
- Where are first aid kits and defibrillators stored?
- Which illnesses and injuries are common to your industry?
“Putting a first aid response team together is not rocket science, but at the same time, there is no cookie-cutter approach, because every facility is going to be different,” Rehberg said. “The needs are going to be different. Just the size and uniqueness of the campus is going to be different, so it really does take a little bit of planning by all the stakeholders involved.”
Associate Editor Kevin Druley discusses this article on the September 2022 episode of Safety+Health's “On the Safe Side” podcast.
Look at OSHA regulations
Several OSHA standards contain first aid requirements, including occupation-specific regulations covering construction (1926.500); telecommunications (1910.268); welding, cutting and brazing (1910.252); electric power generation, transmission and distribution (1910.269); logging operations (1910.266); and site clearing (1926.604).
Although OSHA doesn’t provide specific guidance on volunteer first aid response teams, the agency’s standard on medical service and first aid (1910.151) states that “in the absence of an infirmary, clinic or hospital in near proximity to the workplace, which is used for the treatment of all injured employees, a person or persons shall be adequately trained to render first aid.”
OSHA offered more information in a November 1992 letter of interpretation:
“In areas where accidents resulting in suffocation, severe bleeding, or other life-threatening injury or illness can reasonably be expected, a three- to four-minute response time, from time of injury to time of administering first aid, is required. In other circumstances, i.e., where a life-threatening injury is an unlikely outcome of an accident, a 15-minute response time is acceptable.”
Rehberg says that, when you’re determining a worksite’s distance from emergency medical care, take into account that travel time is dependent on weather, traffic, distance and ambulance availability. You’ll also need to allow time for response crews to dispatch and unload equipment.
Create a plan
A comprehensive, venue-specific incident response plan should be the bedrock of any volunteer workplace first aid response team, Rehberg said.
After conducting a risk assessment of the facility, team leaders should form a plan that identifies objectives and goals, fully de-fines the roles of team members in an emergency, and specifies any regulations covered by the plan.
The response plan should be included as part of the organization’s comprehensive emergency response plan and include attributes such as:
- A team roster and contact information
- Floor plans showing team member, AED and first aid kit locations
- A list of responsibilities
- Methods for reporting incidents/emergencies
Regarding how to notify team members about an emergency, Rehberg said the previous norm of making announcements over a building’s intercom has mostly been phased out by cellphone apps. “I think with today’s technology, it’s very easy to be able to summon a first aid team with minimal disruption of the rest of business.”
NSC divides each floor of its headquarters into quadrants, which are listed on floor maps posted near stairwells. This can help team members locate an ill or injured person more quickly after being called into action.
Rehberg also recommends talking with management about budget considerations for training, retraining, and regular supply and equipment checks.
The International Safety Equipment Association encourages employers to inspect first aid kits at least monthly or “after a first aid incident when product is used,” and to disinfect cabinet surfaces regularly. Remember that AED batteries – and the electrode pads that attach to the unit – have an expiration date.
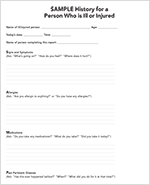
NSC’s in-house first aid kits contain copies of SAMPLE history questions (signs and symptoms, allergies, medications, past pertinent illnesses, last food or drink, and events). If the distressed person is able to talk, team members should ask the SAMPLE questions, then write down the answers to hand to first responders.
Put your team together
Although some workers may believe they can’t be part of a first aid response team because they don’t have a medical background, Prentice said anyone with a passion for assisting others can be trained. She uses NSC’s volunteer team as an example.
“I think there’s always people who want to help out for their colleagues. You just have to find out who they are. But what we really focused on was, we wanted to make sure that everyone felt like they were empowered to be a workplace first responder.”
NSC volunteers complete free training on first aid, CPR, AED and “Stop the Bleed” – which teaches how to curb bleeding resulting from injury. (Learn more at stopthebleed.org.)
Along with the initial training, volunteers are called on to attend quarterly refresher trainings that include simulated medical emergencies. These drills help team members demonstrate their ability to correctly perform first aid, CPR and AED skills.
Talk about duties and expectations
Incidents a team may encounter include diabetic emergencies, severe allergic reactions, airway and breathing emergencies, bleeding, fractures, heart attacks, strokes, shock, and overdoses. Some situations may involve bodily fluids.
Experts say it’s important to ask anyone interested in joining a workplace first aid response team about what scenarios they’re comfortable handling and if they’re willing to perform additional duties.
“Another important role that I think a lot of people forget about is we need people who were comfortable waving down EMS, directing them to the injured or ill employee,” Prentice added.
Also essential: crowd control. When a medical emergency happens, it’s common for onlookers to appear. Team members who aren’t needed to directly provide assistance to the distressed person can help by keeping other people away from the scene.
Privacy is another issue. Team members need to commit to keeping information about the incident – and the distressed person’s medical information and history – confidential. Whether it’s out of curiosity or genuine concern, co-workers often will ask a member of the first aid response team for details about what happened and the person’s condition. Team members need to be ready to say, “I’m sorry, but I can’t give you any information.”
Prentice said NSC training emphasizes putting yourself in the ill or injured person’s shoes: Would you want your personal health information discussed with other employees? “I think it’s human nature to want to know what’s going on if it’s a friend, it’s a colleague, etc., but at the end of the day, we need to let EMS, on-staff medical or volunteer first aid responders do what they were trained to do and give them that respect.”
Co-worker questions should be directed to your organization’s safety director or human resources director.
Talk with your team
Aim to build a team that’s mutually respectful, trustworthy and willing to work together, Rehberg advises. The goal is to bridge the gap between an emergency occurring and EMS’ arrival – to help keep injured or ill people from getting worse until they can receive professional care. Team leaders should reiterate this to team members, and schedule debriefings after major incidents to talk about the response, thank the team for helping, and encourage feedback and discussion.
“You don’t need to be a trained medical professional to save somebody’s life,” Rehberg said.
Post a comment to this article
Safety+Health welcomes comments that promote respectful dialogue. Please stay on topic. Comments that contain personal attacks, profanity or abusive language – or those aggressively promoting products or services – will be removed. We reserve the right to determine which comments violate our comment policy. (Anonymous comments are welcome; merely skip the “name” field in the comment box. An email address is required but will not be included with your comment.)